Thyroid Eye Disease Surgery and Surgical Management


Thyroid eye disease surgery (the surgical management of thyroid eye disease) follows a sequence that is tailored to patient needs and the extent of surgical rehabilitation is likewise customized and patient-specific.
Coordination and proper sequencing of surgical intervention is key to promoting successful outcomes. We focus primarily on orbital decompression and eyelid surgery – the two main reconstructive surgeries performed by oculoplastic surgeons for patients with TED.
Living with thyroid eye disease requires understanding your surgical treatment options, as they play a critical role in protecting your vision and improving your quality of life.
Orbital decompression surgery is performed to address the tight compartment caused by the expansion of orbital soft tissues. The surgery essentially rebalances the contents to the size of the bony orbit, thereby reducing orbital pressure, proptosis, and, when present, compressive optic neuropathy. Surgical techniques include different approaches to removing orbital bone in order to enlarge the space within the orbital compartment, as well as removal of scarred fat and connective tissue to reduce the volume of orbital soft tissue.
With improved techniques and better fellowship training, the trend in surgical decompression has been toward more nuanced customizable techniques that enhance outcomes and decrease morbidity. Each surgery for TED is individually tailored based on patient characteristics and surgeon experience. The goal of surgery is to expand the posterior bony part of the orbit in order to accommodate the fibrotic, thickened muscles while removing abnormal, scarred fat that occupies too much space in the orbit, which pushes the eye forward.
Customization of orbital decompression can be accomplished through the number and choice of orbital walls removed, augmenting the decompression with excision of hypertrophied and fibrotic orbital fat, varying the extent of ethmoidectomy (medial decompression) or deep bone removal (lateral decompression), targeting the posterior inferomedial strut and orbital process of the palatine bone, and timing of surgery.
The development of modern techniques has been made possible by advanced noninvasive imaging, detailed preoperative analysis, stereotactic navigation, piezoelectric technology, and an enhanced understanding of orbital pathology.
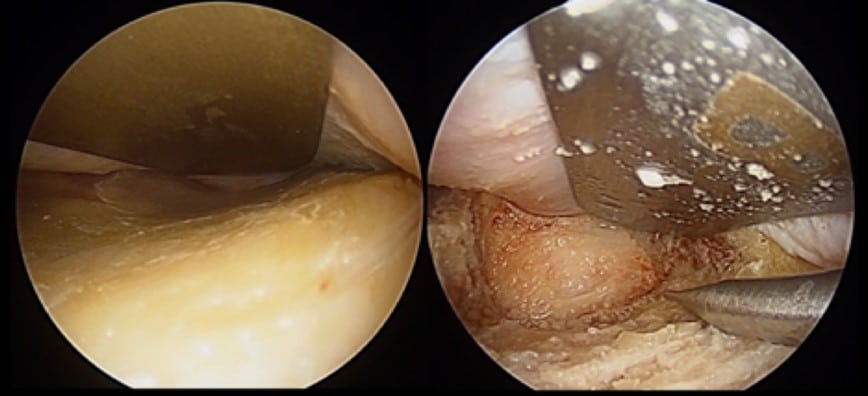
In lateral orbital decompression, once the trigone is exposed, bone removal is performed through the anterior cortical bone to expose the diploic space, which is filled with cancellous bone. Bone removal continues through the diploe, while every effort is made to avoid exposure of dura mater – the lining of the brain. To achieve a maximal decompression, the diploic space should be removed entirely to expose the inner cortical table of bone covering the temporal lobe posteriorly and the frontal lobe superiorly.

Decompression of the orbital floor, whether directly or through inferior extension of a lateral decompression, can lead to inferior globe displacement.
The combination of posterior and inferior displacement of the globe has the secondary effect of reducing lower eyelid retraction while increasing upper eyelid retraction, and can be customized to patients needs and overall surgical plan.
The medial transconjunctival approach to orbital decompression facilitates access to the medial and posterior orbital bones to enable decompression without a skin incision. The surgery also includes opening the sinuses and removing any diseased sinus air cells in order to create additional space for orbital tissues to expand into.
Strabismus surgery is performed following orbital decompression surgery, but prior to eyelid retraction surgery. This sequencing is crucial for optimal outcomes.
Eyelid retraction repair is performed last in the surgical sequence. This timing ensures optimal functional and cosmetic outcomes.
The acute phase of TED is marked by congestive and inflammatory signs, such as chemosis, caruncular edema, eyelid edema, orbital pain and progressive strabismus.
For many years, conventional wisdom ruled that orbital decompression should be avoided in patients in the acute phase of TED, limiting treatment to medical measures, including topical lubrication, salt restriction, head elevation, prism glasses, corticosteroids (oral, intravenous or intraorbital), and low-dose external beam radiotherapy.
However, with the understanding that congestion and inflammation cannot be differentiated based on clinical exam, and the further understanding that orbital congestion leads to venous stasis and accumulation of cytokines within the orbit, our surgeons can perform orbital decompression surgery for orbits with acute-phase signs and symptoms – with excellent results.
TED with imminent visual threat due to dysthyroid compressive optic neuropathy (CON) occurs in approximately 6% of patients and represents a unique, more urgent situation. These orbits will typically require decompression surgery, with the urgency determined by the clinical exam findings.
Importantly, unlike other causes of optic neuropathy, such as microvascular disease, visual field loss from CON is often reversible, revealing a unique resilience in retinal ganglion cells and axons that may have to do with axonal stasis. Still, that resilience should not be tested without important medical reasons, and orbital decompression is often required at the earliest opportunity for optimal outcomes.
In patients whose vision is not acutely threatened, the decision regarding when to perform orbital decompression is more nuanced.
A single pulse of intravenous corticosteroids may serve as a therapeutic trial that can differentiate the inflammatory and congestive processes in the acute phase: inflammatory orbitopathy improves following corticosteroid administration, while congestive orbitopathy is usually unresponsive. Early orbital decompression may have beneficial effects on the overall course of the orbitopathy by relieving the orbital congestion and improving blood flow to orbital tissues in patients with symptomatic orbital congestion. Hence, orbital decompression surgery is no longer relegated to a rehabilitative stage once the disease has become quiescent, but is rather considered a key stage of a multi-step approach to control TED and avoid its more significant consequences.
Since its approval by the FDA, teprotumumab (Tepezza®, Horizon Therapeutics) has become another option for patients with active disease and orbital congestion, in addition to or as an alternative to orbital surgery. Studies have revealed that 60-80% of patients have some response to 24 weeks of teprotumumab infusions, and at least half of these patients have a sustained response.
Although early decompression may be beneficial, orbital decompression surgery should not be undertaken prior to the stabilization of endocrine disease. Conventional wisdom is that the thyroid status is not directly related to the orbit. Our clinical experience, and an extensive nuanced reading of the literature, have revealed that this is not necessarily true. In particular, we have found that in patients who have successfully ceased smoking and whose thyroid function tests are stable prior to (and following) decompression, a primary decompression is frequently successful, with rare need for additional decompressions at a later date. Thus, to obtain the best surgical result, the patient’s endocrine status needs to be normal and stable. Furthermore, the presence of TED is a contraindication for RAI therapy, which may provoke a recurrence or worsening of the orbitopathy.
For fat-predominant TED, excision of scarred fat is a primary mode of orbital decompression, usually accompanied by a limited removal of bone.
On the other hand, for TED associated with scarred, thickened muscles, removal of bone is the primary tool for decompression, with excision of scarred fat serving as an adjunct to improve outcomes.
Importantly, in patients with thick, fibrotic muscles, especially those with limited eye movement, even an excellent decompression may not reduce proptosis all that much because of the stiff EOMs resisting the posterior repositioning of the globe within a decompressed orbit. Hence, proptosis reduction is only one variable when assessing outcomes of orbital decompression surgery, with other variables that include conjunctival chemosis and orbital pressure pain, both of which assess improvement in orbital congestion. Both lateral and medial decompression can achieve a good decompression of the orbital apex.
Because the optic foramen is located within the lesser wing of the sphenoid at the posterior edge of the medial wall, a posterior medial decompression has historically been thought to be the most effective approach to treating CON. However, it has been demonstrated that a full lateral decompression with deep bone removal can be just as effective in treating CON as a medial decompression.
Removal of bone is achieved using instruments that carve, contour and suction bony tissue using either ultrasonic or rotational power. The surgeons of Kahana Oculoplasitc and Orbital Surgery utilize an ultrasonic bone aspirator (Sonopet®, Stryker Corp.) for deep bone removal.
Surgery is performed after the disease has been stable for 6-12 months, except in cases of sight-threatening complications. Timing of surgery is very important for successful outcomes.
Surgical treatment order:
This sequence optimizes final results. Not all patients will require each of these surgeries.
Different approaches include removal of bone, fat, or both to create more space in the orbit. The specific technique is chosen based on each patient’s needs.
Initial healing takes 1-2 weeks, but complete resolution of swelling may take 3-6 months. Final results are typically assessed at 6-12 months post-surgery.
Most patients achieve significant improvement in symptoms and appearance with proper surgical treatment. Planning and timing is an important factor in success, which is generally high with an experienced surgeon.
Your surgeon will provide very specific instructions for post operative care. Following these instructions is necessary for optimal recovery.
Risks include new or worsened double vision, damage to vision or loss of vision, numbness, and possible need for additional procedures. Expert planning with your surgeon can reduce these risks.
Most patients can and will experience significant improvement in appearance after surgery. Speak with your surgeon to establish realistic expectations.
Some patients may require multiple procedures to achieve optimal results. The number and type of surgeries depends on your individual needs.
Most surgical results are permanent, though changes can occur if the disease reactivates. Regular follow-up is required to monitor long-term stability.
Kahana Oculoplastic and Orbital Surgery provides comprehensive, compassionate, individualized care. Our commitment to leading-edge techniques and personalized attention ensures optimal outcomes for each of our patients.
Dr. Kahana has taken special interest in thyroid eye disease throughout his career, having performed research on the molecular underpinnings of this complex disease.
Dr. Kahana is an internationally renowned expert in orbital and ophthalmic plastic surgery.
The providers and staff at Kahana Oculoplastic and Orbital Surgery are known for the care and concern they show toward their patients before, during, and after each procedure. Part of our commitment to innovation includes the opportunity for our patients to participate in clinical trials of novel medical therapies for thyroid eye disease. We also host regular patient-centered forums that help educate, engage and support patients and their families.
The team at Kahana Oculoplastic Surgery specializes in the treatment and management of thyroid eye disease.



Dr. Spadaro explains the timeline of clinical research, Teprotumumab (Tepezza®) development, and current clinical trials for thyroid eye disease.
Dr. Underwood discusses the benefits of an early thyroidectomy for preventing thyroid eye disease from worsening and to stabilize thyroid function more rapidly.