Blepharophimosis Syndrome


Blepharophimosis, or BPES, is typically caused by a mutation in the gene FOXL2, however, other genetic mutations are also known to be associated with this syndrome. FOXL2 is a gene that is expressed in several areas in the body, including the eyelids and ovaries.
Those with the genetic mutation have a 50% chance of passing it on to their offspring. BPES does not impact intellectual development in any way. However, a negative impact on visual development can lead to vision disabilities.
Often, patients will demonstrate a significant “chin-up” position (also known as “ocular torticollis”) in order to see from under the eyelids – a situation that can place significant stress on the neck and back and can delay gross motor development in infants and toddlers.
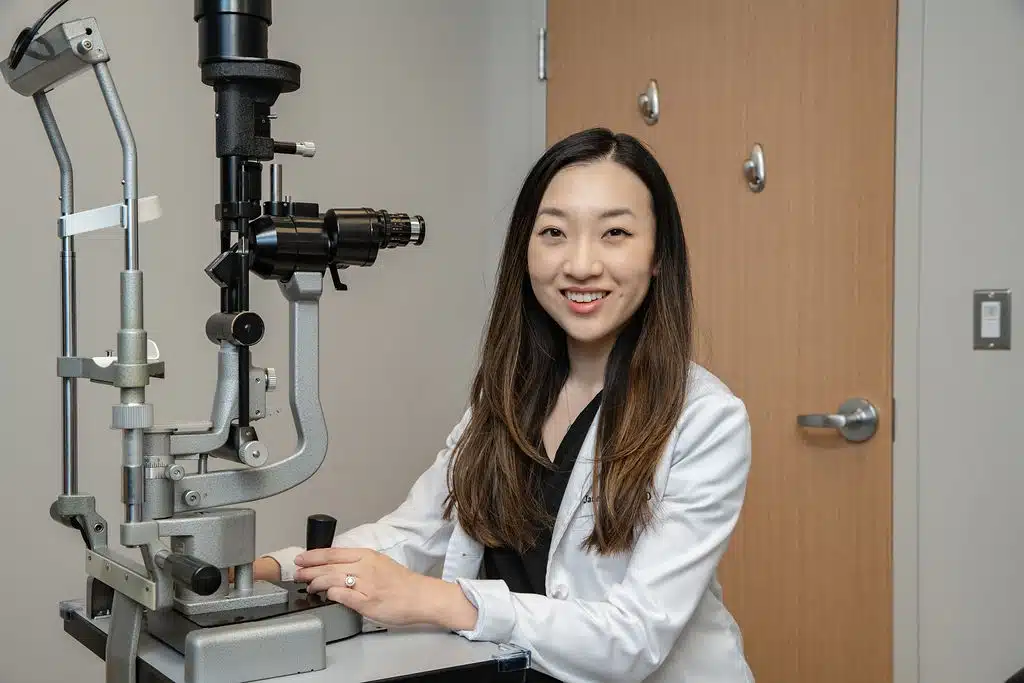
The first and most important step is to have a complete eye exam performed by a fellowship-trained pediatric ophthalmologist.
It is also critical to assess for common but unrelated vision issues, such as strabismus (eye misalignment) and refractive error (the need for glasses). The fact that a child has BPES should not distract from the need to take care of ANY and ALL vision-related issues that commonly arise in young children.
Girls with blepharophimosis syndrome should be assessed by an endocrinologist and gynecologist for potential early menopause and fertility concerns.
It is very important to see a geneticist for genetic counseling, who can help discuss the risk of passing this on to future generations, along with assessing the risk for early menopause.
The primary goal of surgical repair is to facilitate normal development of the visual system and to avoid the consequences of neck strain caused by a “chin-up” position (ocular torticollis).
If visual development is normal, then there is NO REASON to operate on a young child. The ONLY reason to operate on an infant or toddler, in whom surgery is more challenging, is to normalize visual development and/or correct the ocular torticollis. If surgery can be delayed until school age, then it should be delayed in order to optimize long-term results.
Surgery is performed in stages, starting either with the blepharoptosis (to raise the upper eyelid – ptosis correction) or with the epicanthus inversus and telecanthus (to reduce the inner skin folds – medial canthoplasty).
The decision on which surgery to perform first is individualized and takes into account which part of the lid – upper and inner – might be obstructing vision.
The medial canthoplasty is performed by moving skin flaps to reorient the tissues such that the inner skin folds will be pulled inward. In addition, debulking of abnormal medial canthal fat pads is necessary to narrow the nasal bridge to a more anatomically correct position. Care must be taken to avoid injury to the tear drainage (lacrimal) system.
The blepharoptosis repair surgery aims to allow the upper eyelid to elevate better in order to clear the pupil without a chin lift.
There are two methods to correct this, depending on the severity: ptosis repair for those children with good levator muscle function, or a frontalis sling with or without ptosis repair in those with poor levator function. A frontalis sling allows the child to raise their eyelid by activating their brow muscle. To connect the frontalis muscle to the eyelid, traditional surgery utilizes one of several methods: silicone tubing, Gortex suture, connective tissue from the thigh (fascia lata), or cadaveric connective tissue from a tissue bank. After many years of using silicone slings, Dr. Kahana has revised and improved on an old technique in which the frontalis muscle itself is tunneled under the brow and connected to the upper eyelid – forgoing the need for an implant. This technique is called a “frontalis muscle flap sling.” (Credit goes to Dr. Suzana Matayoshi, MD, PhD, Director of Oculoplastic Surgery at the University of Sao Paolo, Brazil, for introducing Dr. Kahana to this approach.)
After surgery, the eyelids will be more open, but they will not close as well when the patient is asleep – at least for the first two to three weeks.
They will also not blink as well because the blinking mechanism is altered by the sling surgery and needs time to recover. Therefore, it is very important that the eyes are kept lubricated – particularly when sleeping. This is done by applying a small amount of eye lubricating ointment to the eyes whenever the child is asleep (including naps). Drying out of the eyes is the most important early complication to avoid – it can lead to corneal infection, scarring and loss of vision.
In infants and pre-verbal toddlers, rubbing of the eyes is often a sign that the eyes are dry and uncomfortable. Fortunately, the issue is usually temporary and improves as the eyelids heal over a few weeks after surgery, although prolonged swelling is possible – particularly with traditional silicone or fascia lata slings.
As long as the eyelids are properly repaired in a timely fashion and there is appropriate follow-up, patients with blepharophimosis syndrome are expected to develop normal vision.
Each patient’s needs are unique and require an individualized approach to treatment.