Ocular Surface Disease


Ocular surface disease (OSD) encompasses a range of disorders affecting the surface of the eye, which consists of the cornea and conjunctiva. These conditions can significantly impact an individual’s quality of life, causing eye irritation, pain, tearing, blurry vision, and even corneal abrasions and infections. Understanding the symptoms, diagnostic methods, and treatment options for OSD is crucial for patients and healthcare providers alike.
The causes of OSD can be divided into several broad groups, some of which can overlap: (1) insufficient or unstable tear film (i.e., “dry eye”), (2) poor epithelial healing related to stem cell dysfunction, (3) poor epithelial healing related to a nerve disorder, and (4) acute or chronic tissue inflammation. Patients can manifest one or more of these groups of conditions and findings, which is what makes treatment of OSD so challenging: many patients require individualized treatment of each factor contributing to their disease.
We perform the following treatments:
Ocular surface disease can manifest through a variety of symptoms, often depending on the specific condition involved. Common symptoms include:
Diagnosing OSD requires a comprehensive eye examination, often involving several tests:
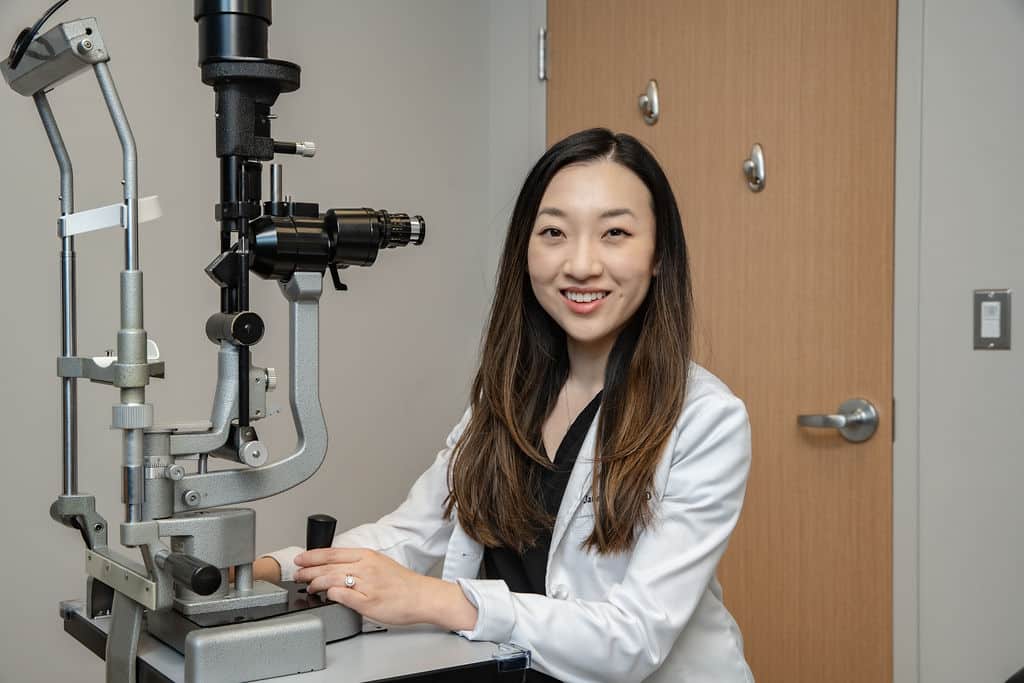
Treatment for OSD varies depending on the underlying cause and severity of the condition. Treatments are generally divided into non-surgical and surgical. At Kahana Oculoplastic and Orbital Surgery, we have expertise in all aspects of OSD therapy, including the most advanced surgical interventions. Contact us if you have any questions.
At Kahana Oculoplastic and Orbital Surgery, we have several surgical tools to improve the signs and symptoms of OSD, often getting at the heart of what’s causing the OSD.
As research progresses, new therapies are emerging:
Ocular surface disease represents a complex set of conditions that require a nuanced approach to diagnosis and treatment. Most patients manifest multiple symptoms that result from multiple causes. In order to achieve a good result with reduction of symptoms, every possible cause of OSD needs to be individually addressed, sometimes sequentially, sometimes simultaneously. At Kahana Oculoplastic and Orbital Surgery, we have a unique combination of skills that covers both the medical and surgical aspects of treatment. We are pioneers in the use of regenerative and reconstructive surgeries to improve eye health. We are proud to be the destination of last resort for patients with OSD refractory to standard therapies.
The cornea – the clear part in the front of the eye – is a unique biological tissue in that it has no blood vessels and is optically clear. The clarity of the cornea is a fundamental aspect of vision; without this clarity, good vision is impossible.
While the cornea lacks blood vessels and mostly obtains its oxygen supply directly from the air, it is very rich in innervation. It is among the most highly innervated tissues in the body, and even minor injuries to the cornea can be terribly painful (e.g. corneal scratch). Fortunately, the cornea is also the fastest healing tissue in the body. The ability of the cornea to heal requires special biological signals from the nerves. This signals – neurotrophic molecules – stimulate the cells of the cornea to divide and reform the damaged tissue.

Neurotrophic keratitis is a disorder in which the cornea has lost its nerves. There are many causes to neurotrophic keratitis, including chronic trauma from dry eyes, chronic inflammation, herpes infection, and even congenital absence of the nerve.
A major medical advance of the past decade has been the development of techniques to reinnervate the cornea. These include both medical (eye drops) and surgical (corneal neurotization). The eye drops (cenegermin-bkbj, known as Oxervate) are most useful when the denervation is distal and fairly recent, caused by chronic dry eyes. Otherwise, surgery is required.
Figures: An intra-operative photo of nerve fascicles recruited to re-innervate the damaged cornea & a graphic representation of Corneal Neurotization
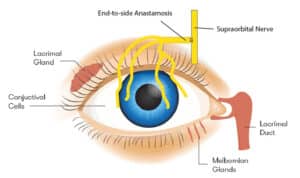
The eye tearing system lubricates and hydrates the eye. The term “dry eye disease” can mean one of two issues. First, aqueous deficient dry eye disease refers to dry eye caused by decreased tear production. Second, evaporative dry eye disease refers to dry eye caused by meibomian gland dysfunction. The signs and symptoms of both affect the entire ocular surface including the tear film, cornea, conjunctiva and eyelids.
Understanding the relationship between dry eyes, ocular surface inflammation, and blepharitis is crucial to treating and maintaining ocular surface health and overall comfort.
Blepharitis refers to inflammation along the base of the lashes and at the meibomian glands along the lid margin. Blepharitis is very common, and people are often asymptomatic for a very long time while the condition progresses. Blepharitis is not a curable condition, however, treatments can alleviate symptoms and prevent the progression of the condition.
Don’t hesitate to get in touch if you have any ocular surface disease questions, concerns or issues.