Thyroid Eye Disease Surgical Management


Surgical management of thyroid eye disease (TED) follows a sequence that is tailored to patient needs.
The extent of surgical rehabilitation is customized and patient-specific. Coordination and proper sequencing of surgical intervention is key to promoting good outcomes. We focus primarily on orbital decompression and eyelid surgery – the two main reconstructive surgeries performed by oculoplastic surgeons for patients with TED.
Orbital decompression surgery is performed to address the tight compartment caused by the expansion of orbital soft tissues.
The surgery essentially rebalances the contents to the size of the bony orbit, thereby reducing orbital pressure, proptosis, and, when present, compressive optic neuropathy. Surgical techniques include different approaches to removing orbital bone in order to enlarge the space within the orbital compartment, as well as removal of scarred fat and connective tissue to reduce the volume of orbital soft tissue.
With improved techniques and better fellowship training, the trend in surgical decompression has been toward more nuanced customizable techniques that enhance outcomes and decrease morbidity.
Dr. Kahana has been a leader in developing customizable minimally-invasive surgical approaches to orbital decompression.
Each surgery for TED is individually tailored based on patient characteristics and surgeon experience. The goal of surgery is to expand the posterior bony part of the orbit in order to accommodate the fibrotic, thickened muscles while removing abnormal, scarred fat that occupies too much space in the orbit, which pushes the eye forward. Importantly, improved understanding of how to deeply contour the diploic spaces within the sphenoid, frontal and zygomatic bones have led to excellent results with dramatic improvements in proptosis reduction through smaller incisions and without damaging the lateral orbital rim.
Customization of orbital decompression can be accomplished through the number and choice of orbital walls removed, augmenting the decompression with excision of hypertrophied and fibrotic orbital fat, varying the extent of ethmoidectomy (medial decompression) or deep bone removal (lateral decompression), targeting the posterior inferomedial strut and orbital process of the palatine bone, and timing of surgery.
The development of modern techniques has been made possible by advancements in noninvasive imaging, preoperative analysis of the orbital anatomy, stereotactic image-guided surgical navigation devices, Piezoelectric technology that minimizes tissue damage, and an improved understanding of the spectrum of orbital pathology represented by thyroid eye disease (TED).
The surgeons at Kahana Oculoplastic and Orbital Surgery utilize ultrasonic aspiration through small incisions to remove bone just where it needs to be removed, minimizing the risk of damage to other parts of the orbit. Frequently, surgery is performed using stereotactic navigation. Dr. Kahana’s research has shown that stereotactic navigation facilitates the small incision approach and actually improves surgical outcomes by improving proptosis reduction and reducing the rates of post-operative strabismus.
Video resource: Cadaver Orbital Decompression Surgery – A Brief Overview by Dr. Alon Kahana
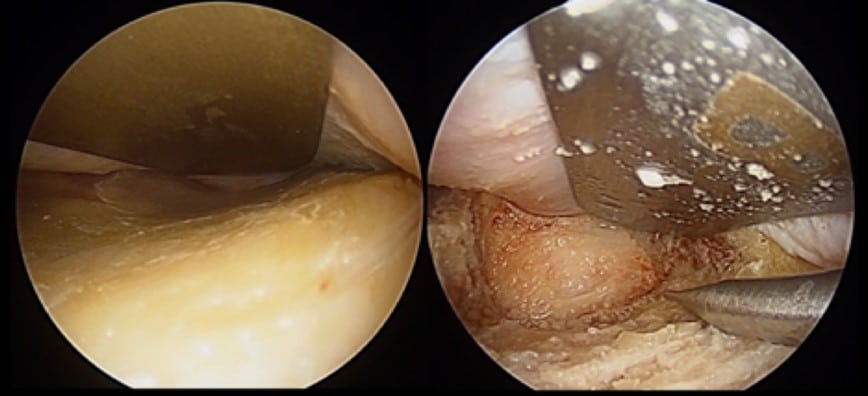
In lateral orbital decompression, once the trigone is exposed, bone removal is performed through the anterior cortical bone to expose the diploic space, which is filled with cancellous bone.
Bone removal continues through the diploe, while every effort is made to avoid exposure of dura mater – the lining of the brain. To achieve a maximal decompression, the diploic space should be removed entirely to expose the inner cortical table of bone covering the temporal lobe posteriorly and the frontal lobe superiorly. In addition to the sphenoid and frontal trigones, significant bone removal can be accomplished along the inferior orbital fissure and extend to the inferolateral orbital floor. Occasionally, the roof of the maxillary sinus may be exposed. Superolaterally, the bone above the lacrimal gland fossa can also be removed.

Decompression of the orbital floor, whether directly or through inferior extension of a lateral decompression, can lead to inferior globe displacement.
The combination of posterior and inferior displacement of the globe has the secondary effect of reducing lower eyelid retraction while increasing upper eyelid retraction, and can be customized to patients needs and overall surgical plan.
Adjunctive fat excision can now be performed, with excellent access to both inferolateral and superolateral fat compartments, and with good effect on both proptosis and lower eyelid contour/fullness.
The medial transconjunctival approach to orbital decompression facilitates access to the medial and posterior orbital bones to enable decompression without a skin incision.
The surgery also includes opening the sinuses and removing any diseased sinus air cells in order to create additional space for orbital tissues to expand into. An important consideration of medial orbital decompression is strabismus, as this technique has been known to be associated with greater degree of induced strabismus. However, Kahana Oculoplastic and Orbital Surgery surgeons have perfected the technique to minimize the risk of induced strabismus and double vision (diplopia). Additional decompression can be achieved at the orbital apex by removing the posterior-most part of the orbital floor – a very effect and safe technique to decompress the optic nerve.
Once the bony decompression is completed, the periorbita is opened sharply with scissors or a sickle blade to allow for soft tissue herniation into the newly created space.
Following orbital decompression surgery, patients are prescribed oral analgesic medication and cold compresses for 3-5 days, along with the usual regimen of incisional care including an antibiotic ointment.
They should be instructed to avoid exertion, bending, or lifting for at least 2-3 days post-operatively – the key time period for post-operative bleeding. Following surgery in the sinuses, nasal saline spray can be prescribed to facilitate healing and reduce post-operative congestive symptoms.
As with any surgery, orbital decompression can be associated with potential complications. The most important and common risks include infection, worsened strabismus/diplopia, and post-operative hemorrhage causing an acute compartment syndrome.
Temporary postoperative hypoesthesia (numbness) has been reported in up to 29% of lateral decompressions and 17% of other bony decompressions. Diligent follow up of patients in the postoperative period is critical in order to detect potential complications and monitor healing.
Strabismus surgery is performed following orbital decompression surgery, but prior to eyelid retraction surgery.
It is important to note that for patients with double vision who require strabismus surgery, the recession of fibrotic inelastic muscles frequently causes worsening proptosis. Therefore, it is important to provide sufficient decompression to account for the expected increase in proptosis following strabismus surgery, and to properly counsel patients.
Eyelid retraction repair is performed last – once proptosis is reduced to an acceptable level, any compressive issues are addressed, and strabismus is resolved.
Upper eyelid retraction repair typically requires the release of eyelid retractors, which undergo fibrosis as part of the orbitopathy process. This can be done via anterior or posterior surgical approaches and may involve the levator muscle, Müller’s muscle, and/or conjunctiva.
Lower eyelid retraction repair frequently requires a spacer graft, which can be autologous (e.g., hard palate, ear cartilage, dermis), allograft or xenograft (e.g., decellularized dermis), or alloplastic material.
Your doctor will describe the diagnostic process for customizing a surgical plan, perioperative planning, surgical techniques, and post-operative considerations.
The acute phase of TED is marked by congestive and inflammatory signs, such as chemosis, caruncular edema, eyelid edema, orbital pain and progressive strabismus. For many years, conventional wisdom ruled that orbital decompression should be avoided in patients in the acute phase of TED, limiting treatment to medical measures, including topical lubrication, salt restriction, head elevation, prism glasses, corticosteroids (oral, intravenous or intraorbital), and low-dose external beam radiotherapy.
However, with the understanding that congestion and inflammation cannot be differentiated based on clinical exam, and the further understanding that orbital congestion leads to venous stasis and accumulation of cytokines within the orbit, our surgeons can perform orbital decompression surgery for orbits with acute-phase signs and symptoms – with excellent results.
TED with imminent visual threat due to dysthyroid compressive optic neuropathy (CON) occurs in approximately 6% of patients and represents a unique, more urgent situation. These orbits will typically require decompression surgery, with the urgency determined by the clinical exam findings.
Importantly, unlike other causes of optic neuropathy, such as microvascular disease, visual field loss from CON is often reversible, revealing a unique resilience in retinal ganglion cells and axons that may have to do with axonal stasis. Still, that resilience should not be tested without important medical reasons, and orbital decompression is often required at the earliest opportunity for optimal outcomes.
In patients whose vision is not acutely threatened, the decision regarding when to perform orbital decompression is more nuanced.
A single pulse of intravenous corticosteroids may serve as a therapeutic trial that can differentiate the inflammatory and congestive processes in the acute phase: inflammatory orbitopathy improves following corticosteroid administration, while congestive orbitopathy is usually unresponsive. Early orbital decompression may have beneficial effects on the overall course of the orbitopathy by relieving the orbital congestion and improving blood flow to orbital tissues in patients with symptomatic orbital congestion. Hence, orbital decompression surgery is no longer relegated to a rehabilitative stage once the disease has become quiescent, but is rather considered a key stage of a multi-step approach to control TED and avoid its more significant consequences.
Since its approval by the FDA, teprotumumab (Tepezza®, Horizon Therapeutics) has become another option for patients with active disease and orbital congestion, in addition to or as an alternative to orbital surgery. Studies have revealed that 60-80% of patients have some response to 24 weeks of teprotumumab infusions, and at least half of these patients have a sustained response.
Although early decompression may be beneficial, orbital decompression surgery should not be undertaken prior to the stabilization of endocrine disease. Conventional wisdom is that the thyroid status is not directly related to the orbit. Our clinical experience, and an extensive nuanced reading of the literature, have revealed that this is not necessarily true. In particular, we have found that in patients who have successfully ceased smoking and whose thyroid function tests are stable prior to (and following) decompression, a primary decompression is frequently successful, with rare need for additional decompressions at a later date. Thus, to obtain the best surgical result, the patient’s endocrine status needs to be normal and stable. Furthermore, the presence of TED is a contraindication for RAI therapy, which may provoke a recurrence or worsening of the orbitopathy.
For fat-predominant TED, excision of scarred fat is a primary mode of orbital decompression, usually accompanied by a limited removal of bone. On the other hand, for TED associated with scarred, thickened muscles, removal of bone is the primary tool for decompression, with excision of scarred fat serving as an adjunct to improve outcomes.
Importantly, in patients with thick, fibrotic muscles, especially those with limited eye movement, even an excellent decompression may not reduce proptosis all that much because of the stiff EOMs resisting the posterior repositioning of the globe within a decompressed orbit. Hence, proptosis reduction is only one variable when assessing outcomes of orbital decompression surgery, with other variables that include conjunctival chemosis and orbital pressure pain, both of which assess improvement in orbital congestion. Both lateral and medial decompression can achieve a good decompression of the orbital apex.
Because the optic foramen is located within the lesser wing of the sphenoid at the posterior edge of the medial wall, a posterior medial decompression has historically been thought to be the most effective approach to treating CON. However, it has been demonstrated that a full lateral decompression with deep bone removal can be just as effective in treating CON as a medial decompression.
Removal of bone is achieved using instruments that carve, contour and suction bony tissue using either ultrasonic or rotational power. The surgeons of Kahana Oculoplasitc and Orbital Surgery utilize an ultrasonic bone aspirator (Sonopet®, Stryker Corp.) for deep bone removal.