Dry Eye and Blepharitis


Dry eye disease is a condition that affects the surface of the eye and hence falls under a category called ocular surface disease (OSD). This broader category encompasses a range of disorders affecting the surface of the eye, which consists of the cornea and conjunctiva.
These conditions can significantly impact an individual’s quality of life, causing eye irritation, pain, tearing, blurry vision, and even corneal abrasions and infections.
It is often associated with inflammation of the eyelid margin (blepharitis), dysfunction of the eyelid oil glands (meibomian gland dysfunction), and infections of the eyelid margin (alternately called a stye, hordeolum or chalazion, depending on specific features). Understanding the symptoms, diagnostic methods, and treatment options for OSD is crucial for patients and healthcare providers alike.
Protection of the eye surface is a complex process. It includes preventing foreign matter from getting to the eye, lubricating the eye, hydrating the eye, and keeping it oxygenated.
The eyelids protect the eye surface from foreign matter, and the tear system lubricates and hydrates the eye. Understanding the relationship between dry eyes, ocular surface inflammation, and blepharitis is crucial to treating and maintaining ocular surface health and overall comfort.
When one of the above components stops working correctly, the eye becomes dry and irritated, leading to redness and inflammation, tear film instability, and irregularity of the ocular surface.
Disruption of these components is also the most common cause of tearing (the other main cause of tearing is obstruction of tear drainage). When the eye is irritated or dry, the nerves of the eye surface send a signal to the tear glands to produce extra tears to address the irritation – more tears than the tear drainage system can handle. Think of tearing that occurs when something is in your eye!
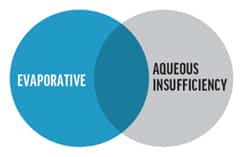 The term “dry eye disease” can relate to both aqueous deficient and evaporative dry eye.
The term “dry eye disease” can relate to both aqueous deficient and evaporative dry eye.The signs and symptoms of both affect the entire ocular surface including the tear film, cornea, conjunctiva and eyelids. To complicate things, symptoms of each condition are often the same, and there is much overlap between the two etiologies. Only about 10% of dry eye disease cases are strictly caused by aqueous deficient dry eye, and the remainder are caused by either evaporative or mixed dry eye disease. It is important to understand the leading causes of both types of dry eye disease.
Aqueous deficient dry eye is caused by decreased secretion of watery tears from the lacrimal gland (think of the three components of the tear film), as seen in cases of aging and drying conditions such as Sjogren’s syndrome, rheumatoid arthritis, radiation to the head and neck that destroys lacrimal gland tissue, or a history of ocular scarring disorders.
Other factors such as decreased corneal sensation or damage to the cornea caused by refractive or cataract surgery can lead to aqueous deficient dry eye disease.
Common treatments of strictly aqueous deficient dry eye disease would include replacement therapy with lubricating eye drops, use of cyclosporine drops such as Restasis or Cequa, Xiidra, biological tear substitutes in the form or autologous tears, or punctual plugs and punctual occlusion.
Evaporative dry eye is more common and is caused largely by inflammation and plugging of the meibomian glands (the oil glands along the lash line), leading to rapid loss of the tear film and irritation from decreased lubrication.
This is called “meibomian gland dysfunction,” or “blepharitis.” Evaporative dry eye disease also includes inflammation of the conjunctiva (conjunctivitis), which is often caused by allergies or chronic irritation of the conjunctiva such as in the case of floppy eyelid syndrome, where the ocular surface is being chafed by the back of your eyelid.
Each of these problems can result in irritated eyes and go through cycles of excess tearing. Treatment should focus on the cause.
Blepharitis refers to inflammation along the base of the lashes and at the meibomian glands along the lid margin. Blepharitis can be split into two subtypes: anterior and posterior. It is important to note that blepharitis is very common, and oftentimes people are asymptomatic for a very long time while the condition is progressing. Blepharitis is not a curable condition, however, treatment aims to alleviate symptoms and prevent progression of the condition.
Anterior blepharitis occurs due to bacteria (staphylococcal) and dandruff of the scalp and eyebrows (seborrheic). These are common skin bacteria and skin conditions, however, both can cause inflammation or infection at the base of the lashes.
Additionally, allergies or a mite (demodex) infestation can cause anterior blepharitis. Again, demodex are very common and these mites feed on the natural bacteria at the lash lines, but when they are overpopulated, this can cause further inflammation and lead to symptoms of itching, redness and irritation at the lid margins.
Oftentimes, anterior blepharitis causes flaky debris and crusting along the lash line, and sometimes it can cause ulcerating sores on the eyelid and lash loss. Maintenance therapy for anterior blepharitis includes proper lid hygiene in the form of regular lid exfoliation with over-the-counter blepharitis wipes or hypochlorous acid sprays, frequent washing of bedding, limiting makeup use, or prescription ointment applied to the lash lines. Lubricating eye drops can help with symptoms of dry eye and ocular irritation.
Posterior blepharitis is what is termed “meibomian gland disease” because this occurs when the meibomian glands along the lid margin become inflamed and oil production (a natural healthy part of the tear film) is disrupted.
The oil within the glands either gets blocked or comes out thick and crusty, further irritating the eye and leading to an unstable and quickly evaporating tear film. Over time, the meibomian gland structure changes or dies off, leading to even worsening symptoms including dry eye disease. Meibomian gland dysfunction can be correlated with rosacea, and is sometimes termed “ocular rosacea.”
Maintenance therapy should include routine hot compresses followed by lid expression (a microwavable moist heat mask such as Bruder mask is recommended), lubricating eye drops, omega-3 dietary supplementation, prescription ointment applied at bedtime and oral doxycycline.
Sometimes, blepharitis and meibomian gland plugging cannot be sufficiently treated using warm compresses and other maintenance therapies. At Kahana Oculoplastic Surgery, we offer in-office thermal pulsation called iLux therapy, as well as an exfoliation of the eyelids called BlephEx. This is an excellent jumpstart to therapy, and patients typically feel symptomatic relief within two to four weeks of treatment. It is best to begin treatment as soon as blepharitis is identified, even if there are minimal symptoms. In cases where the blepharitis is too severe and minimal meibomian glands remain, we offer in-office procedures such as injection with 5-fluorouracil.
What are “stye” and “chalazion”?
When meibomian gland plugging leads to a pocket of infection, it is called a “stye.” When the plugging leads to condensing inflammation, it is called a “chalazion.”
These are treated with aggressive use of hot compresses, injection of 5-fluorouracil, or a procedure to lance and scrub out the swollen pocket of inflammation. Once this is performed, patients need to continue using hot compresses and eyelid margin scrub to keep the meibomian glands unplugged.
Ocular surface disease can manifest through a variety of symptoms, often depending on the specific condition involved.
Treatment for OSD varies depending on the underlying cause and severity of the condition. Treatments are generally divided into non-surgical and surgical. The mainstay treatment of dry eye disease is lubrication of the ocular surface with liquid, gel and salve lubricants.
These are over-the-counter medications that directly address the lack of sufficient fluid on the surface of the eye. We generally recommend either preservative-free lubricants or lubricants that are preserved with mild preservatives, such as boric acid (which dissipates on contact with the ocular surface).
At Kahana Oculoplastic and Orbital Surgery, we have several surgical tools to improve the signs and symptoms of dry eye disease, often getting at the heart of what’s causing the condition.
Eyelid conditions such as ectropion (outward turning) or entropion (inward turning) lead to poor protection of the cornea and conjunctiva, poor distribution of tears, lashes rubbing against the cornea, and keratinization of the conjunctiva on the inside of the eyelid (palpebral conjunctiva). Think of the eyelids as being the windshield wipers, and the eye surface as the windshield. If the wipers work poorly, they leave streaks on the windshield that interfere with the view. Likewise with the cornea – if the eyelid blink is poor and the eyelids are poorly fitting, the cornea develops irregularities that interfere with vision. Correcting the eyelid position can improve eye protection, reduce pain and tearing, and visual function. Beyond standard surgical treatments, Dr. Kahana has developed novel techniques that maximize the eyelid’s protective functions.
Conjunctivochalasis is a condition in which the skin of the eye becomes thickened, diseased, and starts rolling over itself with every blink. Each blink should be a smooth movement of the eyelid over the ocular surface. But with conjunctivochalasis, the blink causes the conjunctiva to rub abnormally against the rest of the eye, causing chronic irritation. Identifying and excising the abnormal conjunctiva and reconstructing the eye tissues can greatly improve eye symptoms.
Ultra-thick amniotic membrane can be sutured onto the surface of the eye to promote regenerative healing of the cornea and conjunctiva. Often the eye needs to be sutured shut for 3-4 weeks while the tissues heal, so this treatment is performed one eye at a time.
Sometimes the tear drainage system is blocked or damaged, leading to excessive tearing. In some cases, this contributes to chronic inflammation and even infection of the eye surface, manifesting as mucoid discharge and eye redness. Reconstructive surgery can restore the function of the lacrimal drainage system to improve tear flow and ocular surface health.
At Kahana Oculoplastic and Orbital Surgery, we are pioneers in the reinnervation of the cornea using nerve grafting. This is a nerve microsurgery performed under a neurosurgical microscope. We have the most experience with this procedure in the Midwest, but success rates exceed 80% in achieving stabilization of the cornea. Please see section on Neurotrophic Keratitis.
As research progresses, new therapies are emerging:
This Dry eye disease represents a complex set of conditions that require a nuanced approach to diagnosis and treatment. Most patients manifest multiple symptoms that result from multiple causes. In order to achieve a good result with reduction of symptoms, every possible cause of dry eyes needs to be individually addressed, sometimes sequentially, sometimes simultaneously. At Kahana Oculoplastic and Orbital Surgery, we have a unique combination of skills that covers both the medical and surgical aspects of treatment. We are pioneers in the use of regenerative and reconstructive surgeries to improve eye health and reduce the symptoms of dry eye disease.
If you suffer from any of these conditions, please call us for an evaluation. We will help identify the cause of your dry eye and treat appropriately.